News & Events
Wave 2: Module 4: Carotid, Vascular access and Venous – Week 1 – Case 2
- September 10, 2025
- Posted by: admin
- Category: Uncategorized
Week 1 – Case 2
56 yrs old right-handed patient known with hypertension, ex-smoking and atrial fibrillation for which he is
taking Apixaban 5mg twice daily. He presented to the neurologist with 2-day history of sudden blackout in the
right eye, slurred speech and left arm weakness that lasted 10 minutes and then resolved completely. Brain
MRI showed multiples areas of infarction in both occipital, Rt parietal and both frontal area of the brain.
Carotid doppler scan showed Rt ICA 50-59% stenosis (PSV 130 cm/s) and Lt ICA 30% stenosis (PSV 89). The
neurologist commenced the patient on Atorvastatin 80 mg once daily and referred him to you for
consideration of carotid endarterectomy?
Q1: How will you manage this patient? Please justify your answer.
Q2: Are there any further tests/investigations that can help you make the decision regarding the
management?
Q3: What if the brain MRI did not show any area of infarction, will that make you change your management?
Q1: How will you manage this patient? Please justify your answer.
the patient had ischemic TIA and infarction on both sides despite anticoagulation
in addition he had rt side parietal infarction on the same territory of rt ICA
Patient is indicated for CEA
Q2: Are there any further tests/investigations that can help you make the decision regarding the management?
CT angio of aortic arch and great vessels
echo and transesophageal echo to exclude PFO or left atrial appendage thrombus
TCD to exclude ipsilateral embolism
Q3: What if the brain MRI did not show any area of infarction, will that make you change your management?
yes
one attack of TIA with no recurrence with other cause than atherosclerosis stenosis of ICA which is Atrial fibrillation
no indication for CEA and we will go for RF control , lifestyle advice and , clopidogreal 75 mg and statin
A1: Symptomatic ischemic TIA with small infarcts, cardiac or carotid source. Stenosis <60% → BMT + RF modification, follow-up, no surgery if symptoms not recurrent (ESVS).
A2: Cardiac work-up: ECG, Echo, TEE.
A3: Non-recurrent, <60% stenosis → BMT only, no CEA/CAS.
A1:
According to the presentation history and MRI findings the ptn had symptomatic ischemic TIA with brain infarctions could be cardiac or carotid source
In ptn with symptomatic <60% carotid stenosis BMT with RF modification and follow up the patient with no surgical intervention as far as the symptoms are not recurring according to the ESVS guidelines
A2:
ECG ECHO TEE for the cardiac source
A3:
As long as it is not recurrent or asymptomatic less than 60% so BMT alone with no need for CEA or CAS
Q1
This patient has carotid stenosis > 50% with AF and multiple vascular territory affected, so mostly from cardiac source
so i will continue the anticoagulant and I will add the BMT for carotid stosis
“if the event happens again, i will consider CEA”
Q2
yes in this case we can’t depend on the doppler alone CTA is essential, also i will request Echo searching for cardiac thrombus
Q3
no it will not change my management plan
A1)
Continue Apixaban 5 mg BID
Continue Atorvastatin 80 mg (target LDL <55 mg/dL).
Strict BP control (<130/80 mmHg).
Lifestyle changes: smoking cessation, diet, exercise.
Follow-up carotid duplex in 6–12 months
As source is cardioembolic source Dt AF
…………
A2)
Neurovascular Imaging : CTA or MRA neck & brain → confirms carotid stenosis and evaluates intracranial vessels.
Cardiac Evaluation: Transthoracic or Transesophageal Echo → check for: Left atrial thrombus, valvular lesions.
Blood tests: Lipid profile, HbA1c. Hypercoagulability screen if recurrent infarcts despite anticoagulation.
………………..
A3) Even with a normal MRI, management does not change. Continue medical treatment
CEA/CAS is not indicated unless stenosis ≥70% or recurrent ipsilateral TIAs.
Q3: What if the brain MRI did not show any area of infarction, will that make you change your management?
*if the brain MRI shows no evidence of infarction, this means the patient had a Transient Ischemic Attack (TIA), not a completed stroke.
The patient remains symptomatic because TIA is defined by clinical symptoms, not imaging findings.
*Even with a normal MRI, management does not change. Continue medical treatment
CEA/CAS is not indicated unless stenosis ≥70% or recurrent ipsilateral TIAs.
Q2) Are there any further tests/investigations that can help you make the decision regarding the
management?
*Neurovascular Imaging : CTA or MRA neck & brain → confirms carotid stenosis and evaluates intracranial vessels.
*Cardiac Evaluation: Transthoracic or Transesophageal Echo → check for: Left atrial thrombus, valvular lesions.
*Blood tests: Lipid profile, HbA1c. Hypercoagulability screen if recurrent infarcts despite anticoagulation.
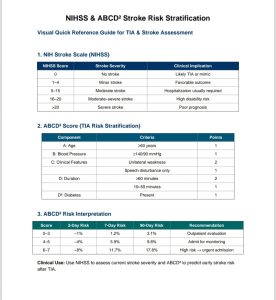
*Risk Stratification: NIH Stroke Scale (NIHSS) and ABCD score for prognosis.
Q1)How will you manage this patient?
(Based on AHA/ASA & ESVS 2023 guidelines)
*Summary of the Case
56 yrs old, risk factors: HTN, ex-smoker, atrial fibrillation (on Apixaban)
Presented with TIA-like symptoms, Brain MRI: Multiple bilateral infarcts → suggests cardioembolic source.
Carotid Doppler: Rt ICA 50–59% stenosis (PSV 130 cm/s) ,Lt ICA 30% stenosis
*guideline-Based Management
According to AHA/ASA and ESVS 2023:
Carotid Endarterectomy (CEA) is recommended only if:
1-Symptomatic patients + ≥70% stenosis (Class I).
2-CEA can be considered for 50–69% symptomatic stenosis only if:
Stroke/TIA symptoms are ipsilateral to the stenosis,No other cause of stroke is found,Surgical risk <6%.
In this case:
Stenosis is moderate (50–59%). Infarcts are bilateral, not confined to right ICA territory.
Patient has atrial fibrillation → strong cardioembolic source.
Already anticoagulated with Apixaban.
➡ Conclusion:
No CEA or carotid stenting at this stage.
Management = Optimal medical therapy
Recommended Plan
Continue Apixaban 5 mg BID
Continue Atorvastatin 80 mg (target LDL <55 mg/dL).
Strict BP control (<130/80 mmHg).
Lifestyle changes: smoking cessation, diet, exercise.
Follow-up carotid duplex in 6–12 months